Blood concentration of NfL showed a statistically significant 93% reduction in change over 12 months in participants receiving HMTM at a dose of 16 mg/day relative to the control group, which correlated significantly with a tau biomarker (p-tau 181) in blood.
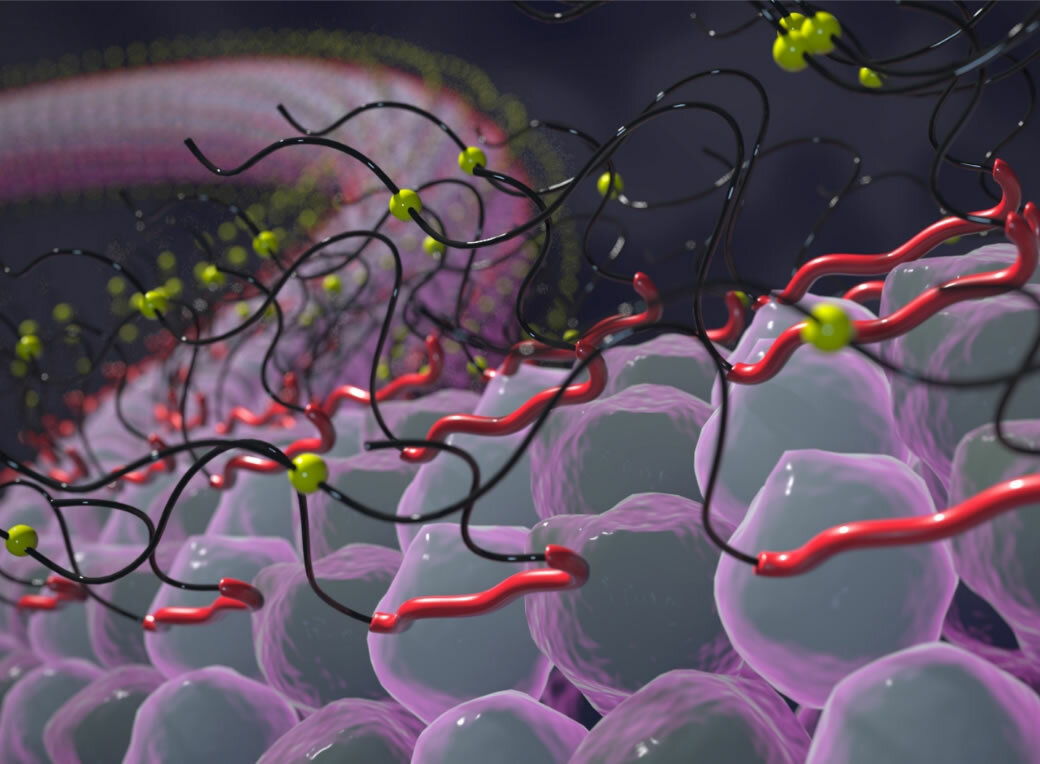
Neurofilaments and tau proteins are essential for neuronal structure and function in the brain. In AD, tau protein aggregates to form toxic fibrils, which damage neurons. The extent of this damage can be measured by the amount of leakage of neurofilament protein into the bloodstream. NfL concentration in blood is known to correlate with tau pathology, disease severity, and therefore cognitive decline and brain atrophy in AD. HMTM, a tau aggregation inhibitor, was designed to reduce tau pathology in AD. Changes in NfL concentration by HMTM indicate a direct impact on disease pathology.
“NfL is a well-studied biomarker with wide applicability to different neurological disorders, including AD,” said Henrik Zetterberg, Professor of Neurochemistry, UCL Queen Square Institute of Neurology. “Clinical practice has been waiting decades to uncover meaningful advancements to address unmet needs of people with AD. These new results further support the importance of NfL as an AD biomarker both for diagnosis and measurement of treatment effect.”
“The NfL results demonstrate that a drug targeting tau pathology reduces the neurodegeneration that underlies clinical decline in AD,” said Claude Wischik, Executive Chairman, TauRx. “They bring us a step closer to offering an effective new treatment option for people with AD. Because it is taken as a tablet and has a strong safety profile, HMTM would be readily accessible to people needing a disease modifying treatment.”
TauRx will submit the HMTM results from LUCIDITY and earlier trials for regulatory approval in the US, UK and other territories.
For additional information, please visit: https://aaic.alz.org/program/scientific-sessions.asp.
TauRx’s hydromethylthionine mesylate (HMTM) demonstrates significant reduction in neurodegeneration in Alzheimer’s Disease (AD).